which urinalysis finding indicates a urinary tract infection?
Urinary tract infections (UTIs) – an overview of lower UTI management in adults
Lower urinary tract infection (UTI) is one of the nigh common community-acquired infections, with more than half of all females experiencing at to the lowest degree one episode during their lifetime. In the absence of complicating factors, initial empiric antibiotic treatment is usually sufficient in otherwise salubrious, non-meaning, pre-menopausal females with an astute or intermittent UTI, without the need for laboratory sensitivity testing.
Delight login to salve this article.
Published: 10 Dec 2021
Key practise points:
- In most cases, the diagnosis of an uncomplicated lower UTI is guided by clinical symptoms and signs, along with urine dipstick analysis if required
- Empiric antibiotics should exist prescribed for females with an uncomplicated UTI
- Obtaining a midstream urine sample for microscopy, culture and sensitivity assay is generally only recommended in people with UTIs who are at higher hazard of complications, e.grand. males, pregnant females and people with diabetes, recurrent infections, renal failure or a urinary catheter
- Self-care strategies should be discussed with all patients who take a UTI to help reduce the risk of future infections, east.g. sufficient fluid intake, improving hygiene and toileting practices and voiding subsequently sexual intercourse
- Non-antibiotic prophylactic strategies can be considered in patients who feel recurrent UTIs but are not routinely recommended in current guidelines due to depression-quality evidence of benefit
- Antibiotic prophylaxis is highly constructive at preventing recurrent UTIs, however, this should usually only be considered as a "last resort" if other strategies are unsuccessful – primarily due to the hazard of antibiotic resistance
- Patients with asymptomatic UTIs should by and large not be treated with antibiotics; the exception is pregnant females, who should be screened at the first antenatal appointment (via urine culture) and subsequently treated if an infection is identified, regardless of whether symptoms are present
Urinary tract infections (UTIs) are ane of the most common reasons for antibody prescribing in New Zealand.1 The lower urinary tract is nigh oft afflicted due to bacteria, unremarkably from the gastrointestinal tract, entering the urethra and proliferating in the bladder.i When this occurs as a one-off or intermittent infection and remains confined to the urethra and bladder in an otherwise healthy, non-meaning, pre-menopausal female person or male with normal beefcake, it is broadly referred to as an elementary lower UTI (or cystitis).2–4 In contrast, "complicated UTIs" include infections in people with gamble factors that increase the probability of bacterial colonisation, or that decrease the potential efficacy of antibiotic treatment, e.thou. indwelling catheters, pregnancy, renal calculi, immunosuppressive conditions or anatomical abnormalities.two, 3 Despite this terminology, the criteria for distinguishing UTIs as being "unproblematic" or "complicated" varies across the medical literature, and the significance of risk factors – and the potential need for a referral – differs according to the specific person and their clinical history. Ultimately, the focus of UTI direction in any patient is to promptly resolve the infection before information technology ascends via the ureters to involve one or both of the kidneys (pyelonephritis), which is associated with an increased risk of sepsis and multiorgan involvement.2, three
Females have an increased risk of UTI
Females have an increased UTI risk compared with males, predominantly due to the shorter length of their urethra and the shorter altitude betwixt their urethra and anus.five It is estimated that one-third of females take a UTI before age 24 years, and more than 50% have 1 during their lifetime.half dozen In females, the risk of experiencing UTIs can exist greater due to a number of factors, including:5, 7
- Personal hygiene practices, due east.1000. wiping back to front
- Sexual activeness, e.g. high frequency, spermicide or diaphragm employ
- Incomplete voiding, urinary retentivity or other urinary problems
- Vaginal wall prolapse, e.g. cystocoele
- Vulvovaginal atrophy
- Other anatomical abnormalities
- A personal or family history of UTIs (peculiarly in first-degree female family members, i.e. mothers, sisters, daughters)
The cause of uncomplicated lower UTIs is highly predictable
Escherichia coli is the cause in 70 – 95% of all uncomplicated UTIs;3 other possible causative species include Staphylococcus saprophyticus, Proteus spp., Klebsiella spp. and Enterococcus spp.4 Complicated UTIs are besides more than commonly acquired by E. coli, notwithstanding, the range of possible causative species is much broader than for unproblematic infections.3 Although rare in the community, complicated UTIs can occur as the consequence of fungal infection, which is generally associated with Candida species, e.one thousand. in people with an indwelling catheter.1, iv
Simple lower UTIs tin be diagnosed with a high level of confidence in people with a focused history of lower urinary tract symptoms in the absence of complicating factors or red flags (Figure 1). Although subtle or atypical presentations are possible, the combination of ii or more "archetype" features of a UTI – without vaginal irritation or belch in females – generally indicates that a UTI is likely.2 The archetype features of UTI are:two
- New onset dysuria
- Increased urinary frequency
- Increased urinary urgency
- Suprapubic abdominal pain
For instance, 9 out of ten immature females with a history of new onset dysuria and polyuria, without vaginal irritation or discharge, volition have a UTI.3 Less commonly, people with a UTI may present with other features such equally odorous, discoloured or cloudy urine, nonetheless, this tin also occur due to non-infectious causes, e.g. dehydration, diet or renal calculi.two In addition, a UTI cannot be ruled out completely if only a unmarried symptom or sign is present, and farther investigation may be required depending on private clinical circumstances and history (see: "Urinalysis: indications and conclusions").
Physical test is not required but can help exclude differential diagnoses
A concrete examination is not required to clinically diagnose an uncomplicated lower UTI but can exist helpful to ensure systemic features are not present, e.g. measuring temperature and other baseline observations, equally well as an assessment of the abdomen and flank, primarily checking for renal tenderness on palpation that may signal the infection has spread to the kidneys (Figure 1). Pelvic examination is generally unnecessary in females if an unproblematic UTI is suspected; this should just be performed if the patient's suprapubic pain is pregnant, or if an alternative diagnosis is suspected, such as vaginitis, urethritis associated with sexually transmitted infections (STI) or pelvic inflammatory disease or anatomical abnormalities.2, 8
Other demographic-specific considerations
![]() Males. UTIs are rare in males aged less than 50 years, but the take chances increases with age.9 Although the symptoms and signs are generally similar to those observed in females, UTIs in males are commonly associated with genitourinary tract abnormalities such equally prostatic enlargement.nine As a result, it is of import to inquire virtually whatsoever prostate symptoms, features indicative of epididymo-orchitis or a STI, aslope an intestinal examination (and bedside ultrasound, if bachelor) to check for urinary memory.9 If there is a family history of prostate cancer or relevant symptoms, e.g. a weak or altered urine flow, a prostate examination should be performed.nine A referral is non usually required for males experiencing their first unproblematic UTI, but if they accept a subsequent infection then a renal/bladder ultrasound and a non-acute urology assessment should be bundled.9
Males. UTIs are rare in males aged less than 50 years, but the take chances increases with age.9 Although the symptoms and signs are generally similar to those observed in females, UTIs in males are commonly associated with genitourinary tract abnormalities such equally prostatic enlargement.nine As a result, it is of import to inquire virtually whatsoever prostate symptoms, features indicative of epididymo-orchitis or a STI, aslope an intestinal examination (and bedside ultrasound, if bachelor) to check for urinary memory.9 If there is a family history of prostate cancer or relevant symptoms, e.g. a weak or altered urine flow, a prostate examination should be performed.nine A referral is non usually required for males experiencing their first unproblematic UTI, but if they accept a subsequent infection then a renal/bladder ultrasound and a non-acute urology assessment should be bundled.9
![]() People at risk of a sexually transmitted infection. A STI check may exist considered in people with an increased STI risk to exclude conditions such as chlamydia or gonorrhoea every bit a possible cause of symptoms, particularly if vaginal or urethral discharge is reported.3 Risk factors include having a partner with a STI, having ii or more concurrent sexual partners or a new sexual partner inside three months.v
People at risk of a sexually transmitted infection. A STI check may exist considered in people with an increased STI risk to exclude conditions such as chlamydia or gonorrhoea every bit a possible cause of symptoms, particularly if vaginal or urethral discharge is reported.3 Risk factors include having a partner with a STI, having ii or more concurrent sexual partners or a new sexual partner inside three months.v
![]() Older people. Diagnosing a UTI in older people can exist challenging due to the presence of co-morbidities or the use of multiple medicines, which can obscure or resemble UTI symptoms and signs.10 While classic UTI symptoms can frequently be present, atypical features such as acute confusion (delirium), fatigue and anorexia may also occur.ten Urinary incontinence and other non-specific urinary symptoms are relatively mutual in older people, but alone this is not predictive of a UTI.10
Older people. Diagnosing a UTI in older people can exist challenging due to the presence of co-morbidities or the use of multiple medicines, which can obscure or resemble UTI symptoms and signs.10 While classic UTI symptoms can frequently be present, atypical features such as acute confusion (delirium), fatigue and anorexia may also occur.ten Urinary incontinence and other non-specific urinary symptoms are relatively mutual in older people, but alone this is not predictive of a UTI.10
For further data on the diagnosis and management treatment of UTIs in older people, see: bpac.org.nz/BT/2015/July/guide.aspx
Red flags for a complicated UTI
Most UTIs tin be managed in primary intendance. However, the presence of red flags may indicate a more serious situation requiring secondary intendance advice or referral (Figure one).three, viii In detail, pregnant females with suspected pyelonephritis (eastward.thousand. systemic symptoms, fever > 38°C, significant flank, back or suprapubic abdominal hurting) should be immediately referred for an acute obstetric engagement, and their pb motherhood carer contacted due to the increased risk of maternal and fetal complications.xi In addition, people with suspected pyelonephritis and signs of sepsis (e.chiliad. tachycardia, lower than normal claret pressure, increased respiratory charge per unit) ordinarily require referral to secondary intendance for intravenous antibiotics and fluids.
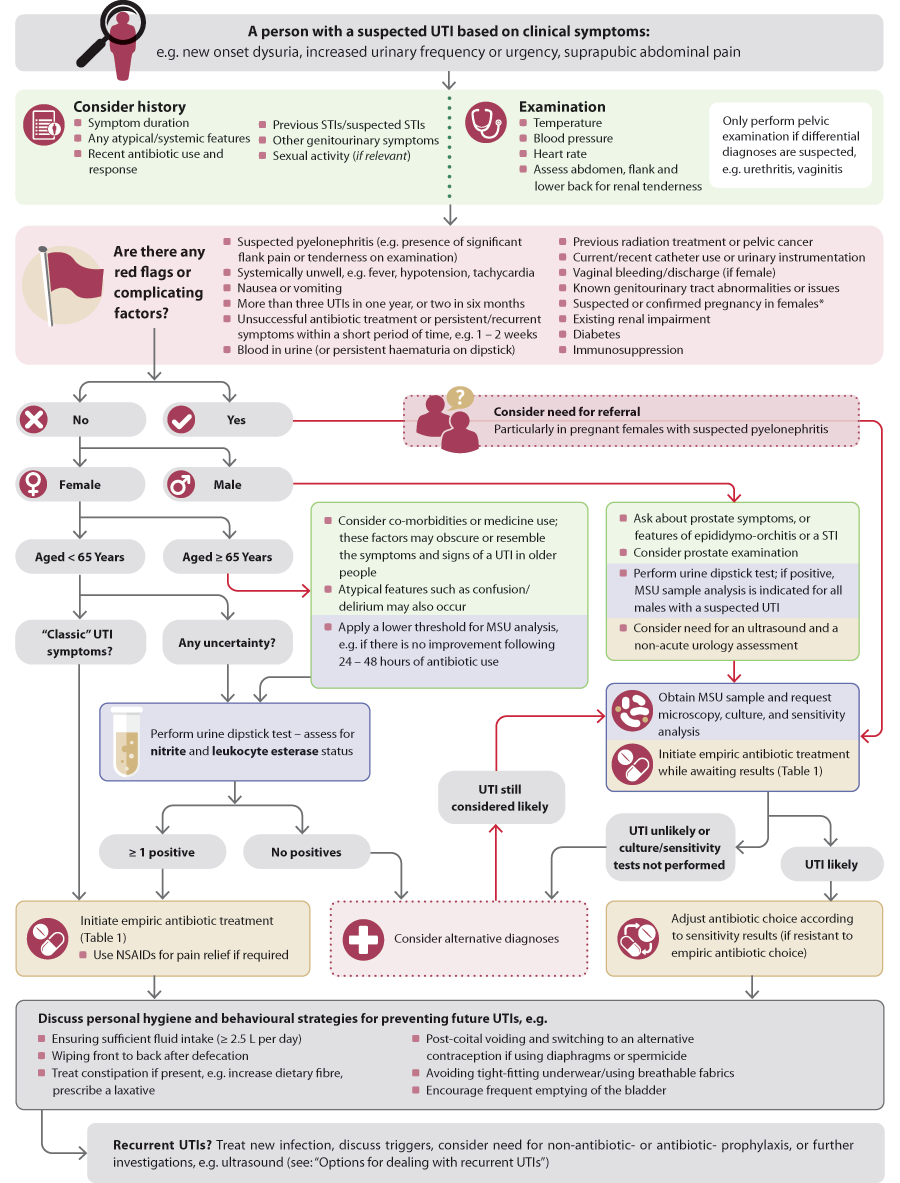
Figure i. The diagnosis and management of symptomatic lower UTIs in adults.2, 8
* A midstream urine (MSU) sample should be obtained, and sent for laboratory analysis in all significant females, ideally every bit part of the first antenatal bank check; asymptomatic bacteriuria should exist treated in this grouping due to the risk of complication
MSU, midstream urine; STI, sexually transmitted infection; UTI, urinary tract infection
Dipstick testing can strengthen diagnostic certainty in symptomatic patients
In most females aged less than 65 years without complicating factors, a lower UTI can exist reliably diagnosed according to the clinical presentation lone, without additional urinalysis. However, if there are singular features, complicating factors or diagnostic uncertainty, then urine dipstick testing tin be useful to indicate if an infection is the probable crusade of their symptoms.2, 8 The fundamental aspects to consider are:2, 12
- Nitrite status – sterile urine by and large should not incorporate detectable traces of nitrite. Well-nigh UTIs are acquired by bacteria belonging to the Enterobacteriaceae family unit, which can metabolise nitrates to nitrites.
- Leukocyte esterase condition – leukocyte esterase is an enzyme produced by white blood cells. If the examination is positive, it may indicate that white blood cells have been generated past the torso in response to infection, and that they are nowadays in the urine (pyuria).
A positive result for either nitrites or leukocyte esterase, in the presence of lower UTI symptoms, is sufficient to ostend a lower UTI diagnosis and go on with treatment.8 All the same, negative results from urine dipstick testing may non reliably exclude the possibility of a UTI, e.g. some UTIs acquired by bacterial species that are unable to produce nitrites, and early pyelonephritis may not produce positive results.8 Haematuria on dipstick can besides be an informative finding every bit this is commonly associated with a UTI only not urethritis.two, iii However, if microscopic haematuria is persistently nowadays in patients with recurrent or ongoing lower urinary tract symptoms, or if gross haematuria is observed (i.e. visible blood in the urine sample), then other diagnoses should be strongly considered, e.g. renal calculi or urinary tract malignancy.2, three
![]() Routine urine dipstick screening for infection in the absenteeism of UTI symptoms (asymptomatic bacteriuria) is not recommended as this should non be treated in patient groups other than meaning females. This is due to the risk of antibiotic-related agin effects, selecting for antibody-resistant bacteria and disruption to the patient's normal urinary microflora.2 Meaning females should be screened via urine culture for asymptomatic bacteriuria, at their first antenatal appointment.
Routine urine dipstick screening for infection in the absenteeism of UTI symptoms (asymptomatic bacteriuria) is not recommended as this should non be treated in patient groups other than meaning females. This is due to the risk of antibiotic-related agin effects, selecting for antibody-resistant bacteria and disruption to the patient's normal urinary microflora.2 Meaning females should be screened via urine culture for asymptomatic bacteriuria, at their first antenatal appointment.
For further information on urine dipstick testing, see: bpac.org.nz/bt/2013/june/urine-tests.aspx
For further information on UTIs and asymptomatic bacteriuria in pregnancy, run into: bpac.org.nz/2019/pregnancy-care.aspx
Requesting analysis of a MSU sample is not routinely recommended
For females with uncomplicated cystitis, the causative leaner and antibiotic sensitivity profile are often predictable. As such, requesting microscopy, culture and sensitivity testing is non necessary as information technology is unlikely to influence treatment decisions (encounter: "Empiric antibiotic choice").ii Obtaining a urine sample – ideally mid-stream urine (MSU) – and requesting laboratory analysis is but indicated in sure circumstances if there is clinical suspicion of a UTI based on symptoms (Figure ane), including:2, 8, 13
- When dipstick testing is negative, but a UTI is yet strongly suspected after considering differential diagnoses
- People with recurrent UTIs, atypical symptoms or persistent symptoms despite antibiotic handling
- People with suspected pyelonephritis
- Females with complicating factors, e.grand. pregnancy, catheterisation, urinary tract abnormalities, immunosuppression, renal impairment, diabetes
- Other high-risk groups, including males, children aged 14 years and under and people living in residential care facilities
Antibiotic resistance is a global effect, primarily driven by inappropriate and excessive use.14 In response, some international guidelines at present recommend that NSAIDs are considered as an alternative first-line handling for UTIs associated with mild symptoms rather than immediate antibiotic use in females aged less than 65 years.ii, fifteen
However, while uncomplicated UTIs tin exist self-limiting in some cases, the natural grade can vary between people, and symptoms may progress instead.xvi Therefore, it currently remains standard practice to prescribe antibiotics to most patients with uncomplicated UTIs in New Zealand primary intendance. A systematic review including ane,309 females with uncomplicated UTI found that the number needed to treat (NNT) with antibiotics rather than NSAIDs to reach symptom resolution in one boosted female past day 3 or 4 of treatment ranged from three to six, i.eastward. more than females take a shorter UTI duration with antibiotic treatment versus NSAID use.17 In add-on, antibiotic use was associated with a lower risk of pyelonephritis and other complications.17
Empiric antibiotic option
The initial antibiotic choice for patients with uncomplicated UTI should be empiric (Table ane).2, 18 If symptoms do not resolve, or a patient experiences a recurrent infection within a short menses of time, e.g. i to ii weeks, consider sending a MSU sample for microscopy, culture and sensitivity assay to guide the selection of an culling pick.2 If laboratory testing is performed at any time, and resistance to the empiric choice is demonstrated, an culling antibiotic can be selected. All the same, MSU samples will not be cultured in some laboratories if the initial microscopy indicates that infection is unlikely, e.g. if white blood cells are absent.
![]() Citrate sodium anhydrous + citric acid anhydrous + sodium bicarbonate + tartaric acid (Ural) is no longer routinely recommended during the acute handling of UTIs every bit information technology raises the urinary pH, which in plow reduces the effectiveness of some antibiotics, e.g. nitrofurantoin.8 Instead, NSAIDs can be considered as an add-on to antibody treatment for pain relief if required.eight
Citrate sodium anhydrous + citric acid anhydrous + sodium bicarbonate + tartaric acid (Ural) is no longer routinely recommended during the acute handling of UTIs every bit information technology raises the urinary pH, which in plow reduces the effectiveness of some antibiotics, e.g. nitrofurantoin.8 Instead, NSAIDs can be considered as an add-on to antibody treatment for pain relief if required.eight
Tabular array 1. Empiric antibiotic regimens for uncomplicated UTI in adults.18
Due north.B. Treat for seven days in significant females and in all males, regardless of antibiotic selection.
| Antibiotic | Dose | |
|---|---|---|
| First-line | Nitrofurantoin*† | Modified release (Macrobid): 100 mg, twice daily, for five days Firsthand release (Nifuran): fifty mg, four times daily, for five days |
| Alternatives | Cefalexin | 500 mg, twice daily, for three days |
| Trimethoprim‡ | 300 mg, in one case daily, for three days |
* Contraindicated in patients with a creatine clearance < 60 mL/min due to the chance of peripheral neuropathy. Prescribe nitrofurantoin by brand proper name to reduce errors equally in that location are two different formulations.xix Nitrofurantoin is not an appropriate showtime-line choice in patients with suspected pyelonephritis as information technology is associated with poor tissue penetration.18
† Avoid subsequently 36 weeks gestation in pregnant females
‡ Avoid in the get-go trimester of pregnancy
Why is trimethoprim no longer a first-line empiric antibiotic option?
Previously, trimethoprim was considered a first-line empiric option for managing uncomplicated UTIs, and it has been usually prescribed past clinicians in main care.i Since 2012, pharmacists who take completed a UTI preparation form have been able to supply trimethoprim without a prescription to females with a suspected UTI aged 16 – 65 years who are not pregnant and do non have whatsoever other complicating factors.twenty
However, there is now evidence that trimethoprim should not be a first-option antibiotic for managing unproblematic lower UTIs due to a growing pattern of resistance beyond New Zealand.21 A multi-region inspect of urine samples obtained betwixt June 2016 and August 2018 demonstrated that approximately one-quarter of all E. coli isolates from females aged 15 – 55 years lacked trimethoprim sensitivity.21 In comparing, < 1% of E. coli tested were resistant to nitrofurantoin, and < 5% were resistant to cefalexin.21 Although trimethoprim is often preferred past people due to its once daily dosing, these findings propose that nitrofurantoin and cefalexin are generally better empiric antibiotic handling choices – unless at that place is recent community resistance data available to pragmatically guide such decisions.
Before the patient leaves the appointment, it is of import to discuss self-care in relation to behavioural and hygiene practices. In some cases, these changes may reduce the hazard of futurity infections, and will likely have wider health benefits.2, 3 Strategies include:
- Ensuring fluid intake is sufficient (at to the lowest degree 2.5 L per mean solar day)
- Avoid wearing tight-fitting underwear and using breathable fabrics such equally cotton rather than synthetics, e.one thousand. nylon or polyester
- Urinating when required (i.e. not "holding on" unnecessarily)
- Post-coital voiding; this behaviour has not been proven to reduce the chance of recurrence in controlled studies, merely is anecdotally supported
- Switching to an culling contraceptive method if diaphragms or spermicide are used (these are associated with an increased risk of UTI)
- Wiping front to dorsum later defaecation or urination to avert perineal or urethral contamination with faecal bacteria
- Treating constipation if present, by increasing dietary fibre intake or using a pharmacological intervention, eastward.chiliad. docusate sodium + sennoside B (Laxsol) or lactulose; constipation may exert pressure on the float, or fifty-fifty obstruct it, leading to incomplete voiding which increases the take chances of a UTI
UTIs are considered recurrent when there are at to the lowest degree 3 symptomatic episodes within 12 months, or ii or more inside six months.3 In near cases, recurrent UTIs are thought to exist caused by reinfection of the urinary tract rather than relapse linked to the previously treated isolate – assuming a complete antibody course was taken.two If the recurrence occurs within a short menstruum of time, e.g. less than two weeks after finishing the antibody course, it is more than likely to be caused by the aforementioned original strain. In these cases, consider obtaining a MSU sample for microscopy, civilisation and sensitivity testing to refine handling selection.3
Not-antibiotic condom treatments can be discussed
In all patients with recurrent UTIs, first reiterate the importance of self-intendance strategies, and investigate known triggers specific to the patient's history, e.g. employ of spermicide-containing contraceptives. Some other non-antibiotic prophylactic strategies that have a depression run a risk of damage can be discussed, but their use is not routinely recommended due to a lack of high-quality evidence for efficacy.2
Condom strategies for UTIs include:two, iii
Topical vaginal oestrogen (estriol; fully funded). The utilise of topical vaginal oestrogen has been found to consistently reduce the take a chance of UTI recurrence in postmenopausal females participating in modest randomised controlled trials. However, given the heterogeneity in the application method used between trials, a pooled estimate of the result size cannot be determined. Oral oestrogen supplementation has not been found to confer a similar benefit in clinical trials.
Consumption of cranberry products, e.k. juices or full-bodied capsules (not funded). Meta-analyses take demonstrated that patients with a history of recurrent UTIs taking cranberry products take a 47% relative risk reduction for future UTIs compared with control groups.22 Yet, there is loftier variability in the "active ingredient" dose betwixt products, inconsistent methodology and driblet-out rates in clinical trials, and no standardised regimen exists. Overconsumption of cranberry products may cause gastrointestinal irritation, as well as exceed the recommended daily carbohydrate intake.
Expert practise tip: when recommending a cranberry product, college percent formulations (e.g. ≥ 18%) are more likely to be effective than lower percentage formulations (east.g. 2 – 4%). Using a higher concentration production besides means that a smaller book or dose can be consumed (east.thou. 200 mL of juice or two capsules, daily). Some people may notice that taking cranberry products at night is more than effective.
Products/supplements containing D-mannose (not funded). D-mannose has been proposed to limit the adherence of leaner to cells in the urinary tract. There is weak prove from unblinded randomised controlled trials that it reduces the risk of UTI recurrence. While these results are encouraging, further investigation is required to decide the optimal dose, frequency and duration of employ.
Lactobacillus containing probiotics (not funded). There is a plausible scientific ground for the utilize of probiotics in preventing UTIs, e.g. the competitive exclusion of UTI-causing bacteria. However, efficacy has non been demonstrated in clinical trials that use oral formulations. The application of Lactobacillus using an intravaginal suppository decreased the rate of recurrent UTIs by 12% compared with placebo in a small clinical trial (Northward = 50).23 However, intravaginal probiotic suppositories for the handling of UTIs are not readily available in New Zealand. If an oral formulation is to be trialled, ensure that i containing Lactobacillus bacteria is used; although there is insufficient clinical trial evidence to guide the selection of a detail Lactobacillus strain or dose, 50. rhamnosus is amongst the well-nigh widely used in clinical trials at doses of ≥ 10viii colony forming units (CFU)/sheathing.24
Low-dose antibiotic prophylaxis should generally be a last resort
Females with recurrent UTIs are over six times less likely to experience another UTI if they accept prophylactic antibiotics.iii However, in keeping with the principles of antibiotic stewardship, this approach is non advisable for all patients; it should generally only exist considered in non-significant females* if behavioural and/or personal hygiene measures are ineffective in preventing recurrent UTIs.19 The main options include a once daily nighttime time dose of nitrofurantoin (immediate release formulation, fifty – 100 mg†), trimethoprim (150 mg) or cefalexin (125 – 250 mg).3, xix Single-dose antibiotic prophylaxis (unapproved indication) may as well exist considered for use after exposure to a known UTI trigger, e.1000. taking a low-dose antibiotic (as above) 2 hours mail service-sexual intercourse.3
There is no convincing evidence on the optimal duration of long-term antibiotic prophylaxis; if it is prescribed, a review should be conducted within iii to half-dozen months to consider the benefits and risks of connected use.ii, three If a decision is made to finish antibiotic prophylaxis, a "back pocket" antibiotic prescription can be provided to manage any acute UTIs that after develop.ii
Methenamine hippurate (Hiprex) 1 1000 every 12 hours tin be considered as an culling form of antimicrobial prophylaxis in patients with a history of recurrent UTIs to avoid long-term antibiotic employ.19 While methenamine hippurate has bacteriostatic properties, information technology is not considered a traditional antibiotic every bit its effect is non-specific; methenamine is progressively converted into formaldehyde within an acidic environment (below a pH half dozen), which then functions to indiscriminately denature bacterial proteins and nucleic acids.25 In near cases, urine is already slightly acidic and hippurate acts to lower the pH further, thereby promoting formaldehyde product.25 The use of methenamine hippurate has been shown to reduce the hazard of recurrent UTIs in several small trials and it is generally well-tolerated in both females and males.2, 25 however, there is non yet sufficient high-quality data to support routine prophylaxis.
*Antibody prophylaxis may also be trialled nether the supervision of a renal specialist (e.chiliad. nephrologist, urologist) in males and pregnant females who experience recurrent UTIs19
†Circumspection is required when considering nitrofurantoin for long-term antibiotic prophylaxis due to the risk of pulmonary toxicity; discontinue if any deterioration in pulmonary function is identifiednineteen
Further investigation for patients with recurrent UTIs
There is no compelling show for early investigation with imaging or cystoscopy in females anile less than 65 years with lower UTI symptoms unless other risk factors are nowadays, east.grand. suspected nephrolithiasis, or if differential diagnoses are strongly suspected.ii Referral for not-acute urology assessment may exist considered in:2, 3, 10
- Females if they continue to present with recurrent UTIs despite sensitivity testing and prophylactic antibiotics, particularly if they have had previous radiation handling or pelvic cancer
- Females with recurrent UTI symptoms, in addition to microscopic haematuria and/or pyuria, despite negative urine cultures; multiple courses of antibiotics should mostly not be used if there is no other show of infection, e.yard. nitrite/leukocyte positivity on dipstick testing
- Males who practice not respond to initial treatment or who experience a second UTI; consider checking for urinary memory past examination or bedside ultrasound in older males
- Older people who practise not improve with antibiotic treatment, fifty-fifty after requesting urine culture to confirm infection and sensitivity analysis to guide antibody selection
For further information on the diagnosis and management of UTIs in other groups:
- Significant females: bpac.org.nz/2019/pregnancy-care.aspx
- Older people: bpac.org.nz/BT/2015/July/guide.aspx
- Children: starship.org.nz/guidelines/urinary-tract-infection/
Acknowledgement
Thank you to Dr David Voss, Nephrologist, Counties Manukau DHB, and Dr Vivian Blackness, Clinical Microbiologist, Southern Community Laboratories, for skilful review of this article.
N.B. Skillful reviewers exercise not write the articles and are not responsible for the final content. bpacnz retains editorial oversight of all content.
References
- Community utilise of antibiotics. Atlas of Healthcare Variation. Wellness Quality & Safety Commission New Zealand. 2020. Available from: https://www.hqsc.govt.nz/our-programmes/health-quality-evaluation/projects/atlas-of-healthcare-variation/community-utilise-of-antibiotics/ (Accessed Oct, 2021).
- Scottish Intercollegiate Guidelines Network (SIGN). Management of suspected bacterial urinary tract infection in adults. 2020. Bachelor from: www.sign.air conditioning.united kingdom (Accessed Oct, 2021).
- McKertich M, Hanegbi U. Recurrent UTIs and cystitis symptoms in women. Aust J Gen Pract 2021;50:199–205. http://dx.doi.org/ten.31128/AJGP-xi-20-5728
- Flores-Mireles AL, Walker JN, Caparon M, et al. Urinary tract infections: epidemiology, mechanisms of infection and treatment options. Nat Rev Microbiol 2015;13:269–84. http://dx.doi.org/10.1038/nrmicro3432
- Storme O, Tirán Saucedo J, Garcia-Mora A, et al. Risk factors and predisposing conditions for urinary tract infection. Ther Adv Urol 2019;eleven:1756287218814382. http://dx.doi.org/10.1177/1756287218814382
- Li R, Leslie SW. Cystitis. In: StatPearls. Treasure Isle (FL): StatPearls Publishing 2021. Available from: http://www.ncbi.nlm.nih.gov/books/NBK482435/ (Accessed October, 2021).
- Scholes D, Hawn TR, Roberts PL, et al. Family history and risk of recurrent cystitis and pyelonephritis in women. Journal of Urology 2010;184:564–9. http://dx.doi.org/10.1016/j.juro.2010.03.139
- Urinary symptoms (UTI) all-time care bundle pathway. Waitemate Commune Health Board. 2017. Available from: https://www.waitematadhb.govt.nz/assets/Documents/wellness-professionals/best-care-bundles/Developed/Urinary-Tract-Infection/UTI-Best-Intendance-Bundle.pdf (Accessed Oct, 2021).
- Bardsley A. Cess, direction and prevention of urinary tract infections in men. Nursing Standard 2018;33:76–82. http://dx.doi.org/ten.7748/ns.2018.e11039
- Godbole GP, Cerruto N, Chavada R. Principles of cess and management of urinary tract infections in older adults. J Pharm Pract Res 2020;50:276–83. http://dx.doi.org/10.1002/jppr.1650
- Urinary tract infection in pregnancy. Due south Australian Perinatal Exercise Guideline. 2021. Available from: https://www.sahealth.sa.gov.au/wps/wcm/connect/4bf52c004eee77c8bfa3bf6a7ac0d6e4/Urinary+Tract+Infection+in+Pregnancy_PPG_v4_0.pdf (Accessed October, 2021).
- Tiso M, Schechter AN. Nitrate reduction to nitrite, nitric oxide and ammonia past gut bacteria under physiological conditions. PLoS I 2015;10:e0119712. http://dx.doi.org/10.1371/periodical.pone.0119712
- Starship. Urinary tract infection. 2020. Available from: https://www.starship.org.nz/guidelines/urinary-tract-infection/ (Accessed October, 2021).
- Antibody resistance. World Health Arrangement. 2021. Available from: https://world wide web.who.int/news-room/fact-sheets/detail/antibiotic-resistance (Accessed Oct, 2021).
- National Institute for Health and Care Excellence (NICE). Urinary tract infection (lower): antimicrobial prescribing. 2018. Available from: https://world wide web.nice.org.uk/guidance/ng109 (Accessed Oct, 2021).
- Hoffmann T, Peiris R, Mar CD, et al. Natural history of uncomplicated urinary tract infection without antibiotics: a systematic review. Br J Gen Pract 2020;70:e714–22. http://dx.doi.org/ten.3399/bjgp20X712781
- Carey MR, Vaughn VM, Mann J, et al. Is non-steroidal anti-inflammatory therapy non-junior to antibiotic therapy in uncomplicated urinary tract infections: a systematic review. J Gen Intern Med 2020;35:1821–9. http://dx.doi.org/10.1007/s11606-020-05745-x
- bpacnz. Antibiotics: choices for common infections. 2017. Bachelor from: https://bpac.org.nz/antibiotics/guide.aspx (Accessed Oct, 2021).
- New Zealand Formulary (NZF). NZF v112. Available from: world wide web.nzf.org.nz (Accessed October, 2021).
- Classification of trimethoprim. Information newspaper for the Medicines Classification Committee. Medsafe. 2018. Available from: https://www.medsafe.govt.nz/profs/class/Agendas/Agen60/5.3.one-MCC-Data-Paper-Trimethoprim.pdf (Accessed Oct, 2021).
- Ussher JE, McAuliffe GN, Elvy JA, et al. Appropriateness of trimethoprim as empiric treatment for cystitis in 15-55 year-erstwhile women: an audit. N Z Med J 2020;133:62–9.
- Wang C-H, Fang C-C, Chen N-C, et al. Cranberry-containing products for prevention of urinary tract infections in susceptible populations: a systematic review and meta-assay of randomized controlled trials. Curvation Intern Med 2012;172:988–96. http://dx.doi.org/ten.1001/archinternmed.2012.3004
- Stapleton AE, Au-Yeung One thousand, Hooton TM, et al. Randomized, placebo-controlled phase 2 trial of a Lactobacillus crispatus probiotic given intravaginally for prevention of recurrent urinary tract infection. Clin Infect Dis 2011;52:1212–7. http://dx.doi.org/10.1093/cid/cir183
- Schwenger EM, Tejani AM, Loewen PS. Probiotics for preventing urinary tract infections in adults and children. Cochrane Database of Systematic Reviews 2015; [Epub ahead of print]. http://dx.doi.org/ten.1002/14651858.CD008772.pub2
- Chwa A, Kavanagh K, Linnebur SA, et al. Evaluation of methenamine for urinary tract infection prevention in older adults: a review of the evidence. Therapeutic Advances in Drug Prophylactic 2019;10:204209861987674. http://dx.doi.org/x.1177/2042098619876749
Made with by the bpacnz team
Source: https://bpac.org.nz/2021/uti.aspx
Posted by: gagnefloore45.blogspot.com

0 Response to "which urinalysis finding indicates a urinary tract infection?"
Post a Comment